Image from: https://www.bonati.com/blog/disc-herniation-healing/
A herniated disc is a spinal condition that affects millions of people worldwide, yet it remains surrounded by misconceptions. Many assume that a disc herniation only happens after a dramatic accident or lifting something far too heavy. In reality, the spine is under pressure every day, and disc injuries can arise from surprisingly ordinary situations.
This blog explores unexpected ways discs can become injured, the most effective treatment options, and what recovery really looks like. We’ll also answer some of the most common questions patients ask about herniated discs—including whether surgery is always required, and if pain is truly lifelong.
Five Unexpected Causes of a Herniated Disc
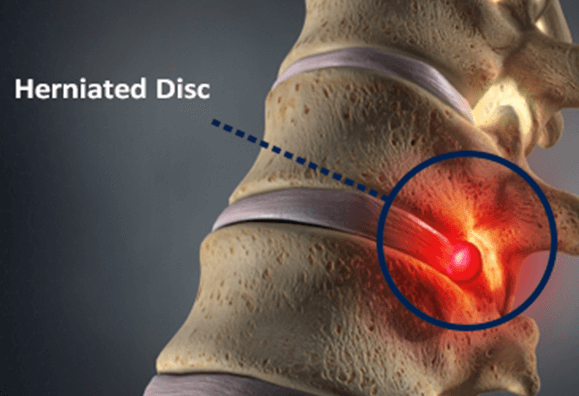
Spinal discs act as cushions between vertebrae, absorbing shock and providing flexibility. A disc herniates when its soft inner core (nucleus pulposus) pushes through a crack in its tougher outer shell (annulus fibrosus). This can irritate or compress nearby nerves, leading to symptoms such as back pain, radiating leg pain (sciatica), tingling, or weakness (Mayo Clinic, 2022). While heavy lifting and acute trauma are common triggers, herniated discs also develop in everyday scenarios:
- Prolonged sitting and poor posture – Sitting for hours in a slouched position places sustained pressure on the lumbar discs and accelerates wear.
- Repetitive twisting motions – Activities like shoveling or swinging a golf club overload the discs when done with poor technique.
- Forceful coughing or sneezing – Sudden spikes in spinal pressure can occasionally cause a vulnerable disc to herniate.
- Carrying asymmetrical loads – Heavy bags or uneven lifting can distort spinal alignment, creating imbalances that stress discs.
- Weak core stability – Without strong abdominal and back muscles, the spine absorbs more impact during daily activities, increasing disc vulnerability.
How Is a Herniated Disc Treated?
The majority of herniated discs improve with conservative management rather than surgery. Standard treatment approaches include (American Association of Neurological Surgeons, 2023):
● Activity modification – Avoiding movements that worsen symptoms while maintaining gentle activity.
● Physiotherapy – Exercises to strengthen the core, restore mobility, and support spinal alignment.
● Heat and cold therapy – To manage pain and inflammation.
● Medications – NSAIDs or prescribed pain relief when necessary.
● Epidural steroid injections – Used in cases of persistent nerve pain to reduce inflammation.
A comprehensive care plan should be overseen by a healthcare professional to ensure safe recovery.
Can You Fully Recover From a Herniated Disc?
Yes—most patients recover fully. Many improve within several weeks, while others may take a few months depending on the severity of the herniation and rehabilitation efforts. Studies show that conservative care leads to significant improvement in the majority of cases (Cleveland Clinic, 2022).
Long-term success relies on:
● Maintaining core and spinal strength.
● Practicing good posture.
● Adopting safe lifting techniques.
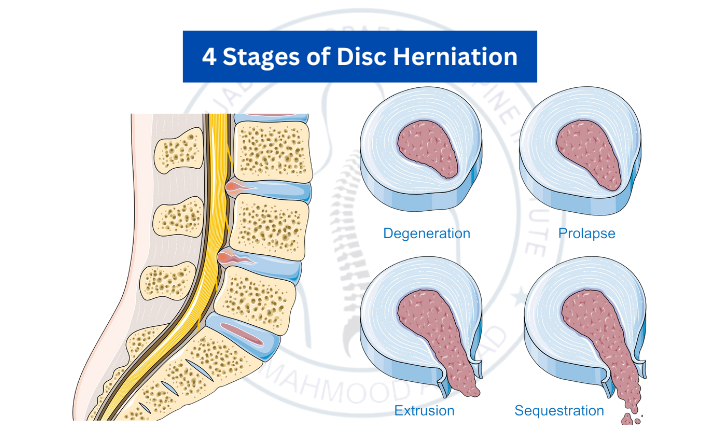
Image from: https://www.bonati.com/blog/disc-herniation-healing/
Is Surgery the Only Option?
Surgery is rarely the first recommendation. It’s usually reserved for patients with severe or persistent symptoms after several months of non-surgical treatment, or for those experiencing significant neurological complications such as weakness or loss of bladder/bowel control (Johns Hopkins Medicine, 2023).
Common procedures include:
● Microdiscectomy – Removing the portion of the disc pressing on the nerve.
● Laminectomy – Removing a small section of bone to relieve pressure on the spinal cord or nerves.
For most people, non-surgical treatment is sufficient and effective.
Will a Herniated Disc Cause Lifelong Pain?
Not necessarily. Many people recover fully and return to daily life without chronic pain. However, recurrent flare-ups may occur if underlying risk factors aren’t addressed. Preventive strategies such as exercise, ergonomic workplace setups, and maintaining healthy body weight greatly reduce recurrence risk (Harvard Health, 2022).
The Bottom Line
A herniated disc can sound intimidating, but it doesn’t automatically mean surgery, lifelong pain, or permanent limitations. With early diagnosis, evidence-based treatment, and lifestyle adjustments, most patients experience significant improvement and even full recovery. By understanding the causes, treatment options, and long-term outlook, you can take active steps to protect your spine and overall health.
Take the Next Step Toward Recovery
If you’re experiencing back pain or suspect a herniated disc, don’t wait for symptoms to worsen. Our team of physiotherapists and chiropractors can provide a thorough assessment, design a personalised treatment plan, and guide you through safe, effective strategies for healing. With the right care, you can reduce pain, restore mobility, and prevent future flare-ups.
References
● Mayo Clinic. (2022). Herniated disk.
● American Association of Neurological Surgeons (AANS). (2023). Herniated Disc.
● Cleveland Clinic. (2022). Herniated Disk.
● Johns Hopkins Medicine. (2023). Herniated Disk.
● Harvard Health Publishing. (2022). Herniated disk.


