What is Shoulder Bursitis?
Bursae are fluid filled sacs that act to reduce friction between bones, tendons and/or muscles surrounding surfaces that are exposed to higher degrees of wear and friction. There are five main bursae that are located around the shoulder that help to provide lubrication and reduce friction during the wide range of movements that the shoulder can do. These include the subacromial-subdeltoid bursa, subscapular recess, subcoracoid bursa, coracoclavicular bursa and supra-acromial bursa.
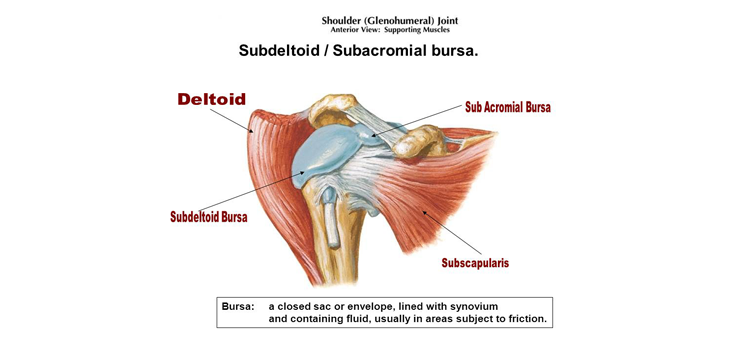
Figure 1. Anatomy of the shoulder with subdeltoid and subacromial bursa locations shown. Note the subacromial bursa lying underneath a bony prominence (acromion) and covering a tendon of a muscle (supraspinatus). Also note the sub-deltoid bursa that closely associates with the sub-acromial bursa and lies between a large muscle (deltoid) and the head of the humeral bone and rotator cuff muscles.
Subacromial-Subdeltoid Bursitis:
The subacromial bursa is located beneath the bony prominence (acromion) at the top of the shoulder and acts to reduce friction between the acromion and tendon of supraspinatus tendon. Usually, the space that lies between the acromion and subacromial bursa is only 1 – 1.5cm in height and is called the subacromial space. The subdeltoid portion of the bursa lies beneath a large muscle called the deltoid which plays a major role in arm movements and shoulder stability. The subdeltoid bursa is so closely associated with the subacromial bursa general inflammation will affect both bursa and thus, they are grouped together.
Subacromial bursitis is the most common form of bursitis that can occur in the shoulder and will commonly cause shoulder pain. Bursitis, regardless of its location, is an inflammatory condition which can have a variety of causes. Subacromial bursitis will often be caused by repetitive overhead activities / overuse, direct trauma (fall), impingement within the subacromial space, infection and autoimmune disease (rheumatoid arthritis).
Typically, individuals who are performing more overhead activities such as athletes (baseball, javelin, cricket etc.) and manual labourers will be at a higher risk of developing shoulder bursits. As people grow older, natural age-related changes can result in the subacromial space becoming smaller and lead to greater impingement within the shoulder joint. Therefore, shoulder bursitis tends to be more common among the older population.
Certain shoulder movements such as repetitive overhead activities, prolonged arm elevation, repetitive shoulder rotation activities, excessive pushing or pulling or sleeping on the affected shoulder, all place compressive forces on the subacromial bursa resulting in irritation, pain and inflammation. Other movements such as abducting the arm (lifting the arm out sideways) can also provide a compressive force that may cause inflammation of the bursa.
Patients that suffer from shoulder bursitis usually experience excessive warmth at the site of the inflamed bursa. They often complain of a great deal of tenderness, pain, and fever. The swelling and redness may spread away from the affected site and go up or down the arm.
Condition Management
Management for Shoulder Bursitis can come through a variety of mediums. Chiropractic and physiotherapy care is the most preferred first line treatment. According to Abdulla et al (2020) supervised progressive shoulder exercises alone or combined with home-based shoulder exercises provided effective short and long-term management for shoulder bursitis. The supervised shoulder therapy and exercise program was provided over 8 weeks and saw improvements across pain (at rest and during movement), quality of life and muscle strength. Pieters et al (2020) also found that these types of shoulder exercise programs provide the same long-term outcomes when compared as a treatment to shoulder decompression surgery for shoulder bursitis / impingement.
Exercises prescribed for shoulder bursitis involve improvement of the muscles that play a role in scapula and shoulder movement. Overall, this aims to improve shoulder stabilising muscles like the rotator cuff as well as scapular stabilising muscles such as Serratus Anterior to improve the quality of movement and reduce impingement around the shoulder. Addition of these scapular stabilising exercises to conventional shoulder strengthening exercises was demonstrated by Shah et al (2014) through a short 4-week program and showed significant improvement in pain and functional status for shoulder bursitis and impingement compared to conventional exercise alone.
In addition to exercise therapy as a treatment for shoulder bursitis, massage and taping have been investigated as adjunct therapies. Haik et al (2016) demonstrated the benefits of massage (manual therapy) in addition to exercise as management of shoulder bursitis. When massage and exercise was compared to exercise alone there was a greater reduction in pain and improvement in function in the short-term. Similarly, Miller and Osmotherly (2009) showed that scapula taping provided a significant reduction in pain during provocative movements for a 2-week period.
Thus, according to current research shoulder bursitis is best managed through chiropractic or physiotherapy care. Exercises should include progressive shoulder strengthening that focuses not only on rotator cuff but also scapula stabilizing muscles. Massage and taping may be used throughout recovery to provide short term pain relief. Finally, completion of at home exercises will enhance the improvements provided by chiropractic and physiotherapy care. This line of care will improve muscle control throughout all shoulder movements to best reduce impingement within the subacromial space and relieve compressing forces from causing inflammation on the subacromial-subdeltoid bursa.
Here at Precision Health we offer services such as Chiropractic care and massage therapy which can aid in your recovery from Shoulder Bursitis. Call (02) 9639 7337 or visit our website to book an appointment now!
References
Abdulla, S.Y. et al. (2015) ‘Is exercise effective for the management of subacromial impingement syndrome and other soft tissue injuries of the shoulder? A systematic review by the Ontario Protocol for Traffic Injury Management (OPTIMA) collaboration’, Manual Therapy, 20(5), pp. 646–656. doi:10.1016/j.math.2015.03.013.
Faruqi, T. and Rizvi, T.J. (2023) Subacromial bursitis, Subacromial Bursitis. Available at: https://www.ncbi.nlm.nih.gov/books/NBK541096/ (Accessed: 25 August 2025).
Haik, M.N. et al. (2016) ‘Effectiveness of physical therapy treatment of clearly defined subacromial pain: A systematic review of Randomised Controlled Trials’, British Journal of Sports Medicine, 50(18), pp. 1124–1134. doi:10.1136/bjsports-2015-095771.
Miller, P. and Osmotherly, P. (2009) ‘Does scapula taping facilitate recovery for shoulder impingement symptoms? A pilot randomized controlled trial’, Journal of Manual & Manipulative Therapy, 17(1). doi:10.1179/jmt.2009.17.1.6e.
Pieters, L. et al. (2020) ‘An update of systematic reviews examining the effectiveness of conservative physical therapy interventions for subacromial shoulder pain’, Journal of Orthopaedic & Sports Physical Therapy, 50(3), pp. 131–141. doi:10.2519/jospt.2020.8498.
Shah, M., Sutaria, J. and Khant, A. (2014) ‘EFFECTIVENESS OF SCAPULAR STABILITY EXERCISES IN THE PATIENT WITH THE SHOULDER IMPINGEMENT SYNDROME’, Indian Journal of Physical Therapy, 2(1), pp. 79–84.
Shoulder bursitis – physiopedia (no date) Shoulder Bursitis. Available at: https://www.physio-pedia.com/Shoulder_Bursitis (Accessed: 25 August 2025).
Book Now With Precision Health today and take the first step towards better health!
Book NowConditions Treated
Take care of your health with precision!
Precision Health Spine & Sports clinic treats a diverse range of neuromuscular and skeletal biomechanical disorders. Whether you are having trouble with your knees, you have a pain in the neck, or if you are just feeling stiff and sore, we can help you with our suite of treatment options that can be tailored especially for you. Take a look at the wide range of disorders we can help you with. Whether you need chiropractic treatment, remedial massage, physiotherapy, podiatry or a combination of disciplines, we have the expertise to decrease your pain and discomfort and increase your mobility and quality of life.
Headaches & Migraines
Shoulder Pain
Elbow Pain
- Ulnar Collateral Ligament Sprain/Strain
- Radial Head Subluxation (Nursemaid’s Elbow)
- Radial Collateral Ligament Sprain/Strain
- Posterior Impingement Syndrome
- Osteochondrosis (Panner’s Disease)
- Olecranon Bursitis (Miner's Elbow)
- Medial Epicondylitis (Golfer's Elbow)
- Little League Elbow Syndrome
- Lateral Epicondylitis (Tennis Elbow)
- Joint Hypermobility Syndrome
- Elbow Joint Dysfunction
Finger and Thumb Pain
Wrist Pain
- Wrist Tendinopathy
- Wrist Ganglions
- Ulnar Tunnel Syndrome (Guyon’s Canal Syndrome)
- Triquetrolunate Dissociation
- Triquetrohamate Instability
- Triangular Fibrocartilage Complex Injury
- Superficial Radial Nerve Compression: Causes and Symptoms
- Scapholunate Dissociation
- Scaphoid Fracture
- Radial Tunnel Syndrome
- Pronator Teres Syndrome
- Posterior Interosseous Nerve Syndrome (PINS)
- Kienbock’s Disease
- Intersection Syndrome
- Hook of Hamate Fracture
- Dorsal Impaction Syndrome
- De Quervain’s Tenosynovitis
- Cubital Tunnel Syndrome
- Carpal Tunnel Syndrome
- Anterior Interosseous Syndrome
Knee Pain
- Tibial Plateau Fractures
- Tennis Leg
- Proximal Tibial-Fibular Subluxation/Dysfunction
- Posterior Cruciate Ligament (PCL) Injury
- Popliteus Tendinitis
- Pes Anserine Bursitis/Tendinitis
- Patellofemoral Pain Syndrome (Runner’s Knee)
- Patellofemoral Arthralgia (Chondromalacia Patellae)
- Patellar Tendinitis (Jumper’s Knee)
- Patellar Dislocation and Subluxation
- Osteochondritis Dissecans (OCD) of the Knee Joint
- Osteoarthritis of the Knee Joint
- Osgood-Schlatter Disease
- Meniscus Injuries to the Knee
- Medial Collateral Ligament (MCL) Injury
- Lateral Collateral Ligament (LCL) Injury
- Knee Joint Dysfunction
- Iliotibial Band Syndrome
- Anterior Cruciate Ligament (ACL) Injury
Head And Neck Pain
- Whiplash Injury (Hyperflexion/Hyperextension Injury)
- Torticollis (Wry Neck)
- Thoracic Outlet Syndrome
- Temporomandibular Joint Dysfunction (TMJ Disorder)
- Herniated Cervical Disc
- Cervical Spondylosis
- Cervical Spine Sprain/Strain
- Cervical Segmental Joint Dysfunction
- Cervical Radiculopathy
- Cervical Facet Syndrome
Back Pain
- Transient-Structural Scoliosis (Sciatic Scoliosis)
- Thoracic Segmental Joint Dysfunction
- T4 Syndrome (Upper Thoracic Syndrome)
- Structural Scoliosis (Idiopathic Scoliosis)
- Shingles (Herpes Zoster Virus)
- Scheuermann’s Disease
- Non-Structural Scoliosis (Postural Scoliosis)
- Kyphosis
- Juvenile Scoliosis
- Infantile Scoliosis
- Compression Fracture
- Adult Scoliosis
Lower Back Pain
- Spondylolisthesis
- Sacroiliac Joint Dysfunction
- Sacroiliac Injury
- Reactive Arthritis (Reiter’s Syndrome)
- Mechanical Low Back Pain
- Lumbosacral Injury
- Lumbar Spondylolysis
- Lumbar Spinal Stenosis (Lumbar Canal Stenosis)
- Lumbar Segmental Joint Dysfunction
- Lumbar Facet Syndrome
- Lumbar Disc Herniation
- Ankylosing Spondylitis
- Abdominal Aortic Aneurysm
Hip, Groin and Thigh Pain
- Trochanteric Pain Syndrome
- Trochanteric Bursitis
- Traumatic Hip Dislocations
- Transient Synovitis
- Stress Fractures (Neck of Femur Fracture)
- Snapping Hip Syndrome
- Slipped Capital Epiphysis (Adolescent Coxa Vara)
- Rheumatoid Arthritis of the Hip Joint
- Quadriceps Muscle Strain/Quadriceps Muscle Tear
- Paget’s Disease
- Osteoarthritis of the Hip Joint
- Osteitis Pubis
- Muscle Contusions/Myositis Ossificans
- Meralgia Paresthetica
- Leg-Calve-Perthe’s Disease (Avascular Necrosis of the Hip)
- Ischial Bursitis
- Iliopectineal Bursitis and Iliopsoas Bursitis
- Hip Fractures
- Hamstring Muscle Injury
- Femoroacetabular Impingement
- Congenital Hip Dislocation (Congenital Hip Dysplasia)
- Adductor Muscle Injury
- Acetabular Labrum Tears